Despite widespread use of the term, anal furunculosis, in the veterinary medical literature, the cutaneous sinus tracts that are the hallmark of this disease do not generally communicate with the rectal lumen (unlike fistulizing Crohn’s disease `in humans). Due to the location and discomfort on examination, dog owners may not be aware of the lesions until they are more advanced. This condition is severely debilitating, causing chronic and often severe pain, open sores, weight loss and diarrhea/straining to defecate in dogs. If not treated appropriately and in a timely manner, the disease can progress to irreversible changes to the rectum and anus and in some cases, ultimately lead to euthanasia due to poor quality of life.
What is the cause of anal furunculosis?
A variety of studies have sought to identify the exact pathogenesis of anal furunculosis but no single cause has been identified at this time. The incidence is highest among German Shepherd dogs (GSD’s), a genetic link is suspected, unfortunately, as of yet the genetic markers have not been identified. Low tail carriage used to be thought a predisposing factor but other affected breeds and lack of resolution with tail amputation have disproven this theory. More recent research suggests an immune-mediated cause with similarities to the human ailment, Crohn’s disease noted.
Which dogs are affected
Age of onset is usually young adult to middle-aged with most patients being 2 to 9 years of age. Although GSD’s are most commonly affected, other breeds diagnosed with this disease include but are not limited to Shih Tzu, Pembroke Welsh corgis, boxers, Labrador retrievers and mixed breed dogs.
Clinical signs of anal furunculosis
Clients most commonly report tenesmus (straining to defecate), hematochezia (blood in the stool), dyschezia (difficultly defecating), frequent small volumes of feces, licking the anus and yellow to white discharge from openings in the skin around the anus (furuncles, sinuses or furuncles). A thorough examination of the rectum and anus will typically reveal painful sinuses, draining tracts and/or ulcerations surrounding the anus. Typically, the lesions around the anus do not communicate with the rectal lumen. Additionally, weight loss, decrease/loss of appetite, lethargy are also often noted.
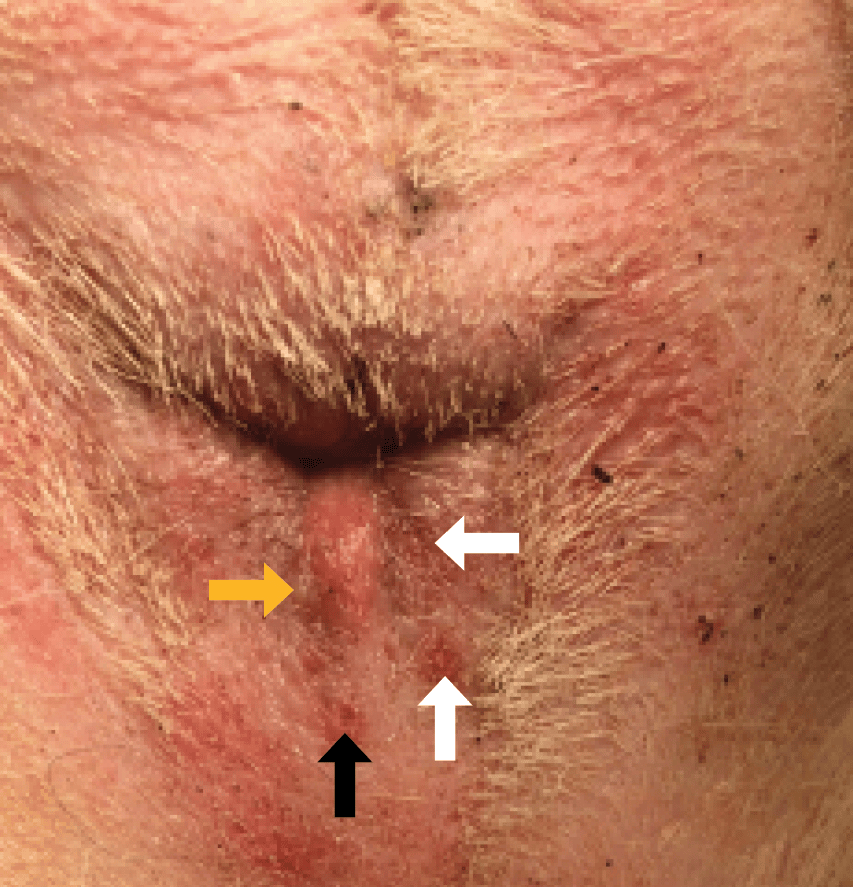
Figure 1. Mild case of anal furunculosis with draining tract (black arrow), erosions (white arrows), and a pustule (yellow arrow)
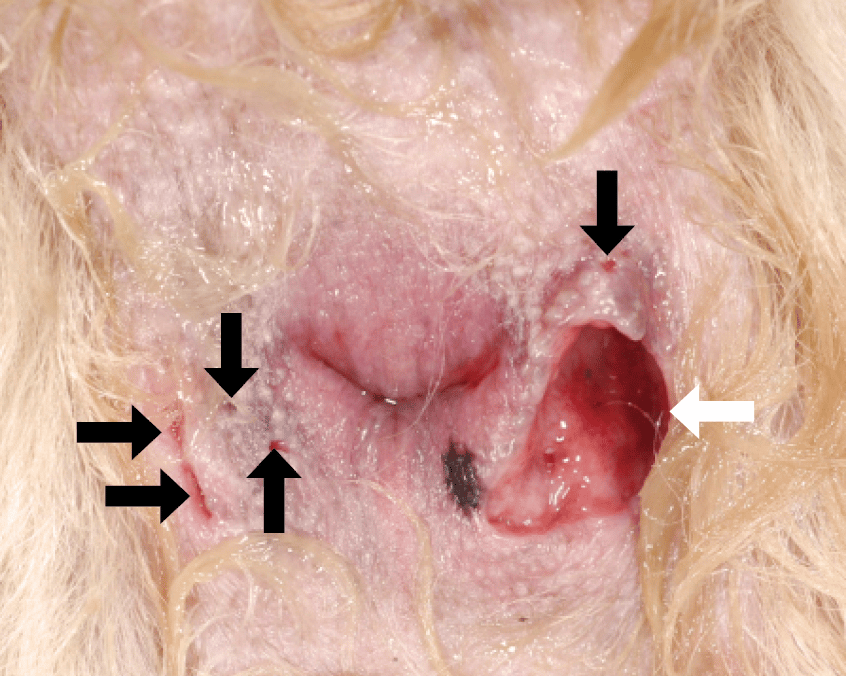
Figure 2. Severe case of anal furunculosis with several draining tracts (black arrows) and a large sinus (white arrow).
Diagnosis of anal furunculosis
Differential diagnoses can vary greatly, depending on the presenting clinical signs. If the only signs noted are perianal pruritus, then other differentials include allergic dermatitis (atopic dermatitis and adverse food reaction) and anal sac abscess. If the patient has tenesmus and hematochezia only (no draining tracts or visible furuncles), the primary differentials become gastrointestinal conditions (e.g., inflammatory bowel disease, intestinal parasites, rectal strictures). If concurrent diseases are not addressed, treatment of the anal furunculosis will not resolve all clinical signs.
As mentioned previously, a thorough rectal examination should be performed to identify any other associated abnormalities in the region. Because of significant pain many patients will require pain medication and sedation before they can tolerate a full rectal examination. Depending on disease severity and duration, rectal examination can reveal a spectrum of findings from nothing abnormal up to severe scarring and constriction or anal stricture. For all patients, thorough palpation and expression of the anal sacs is necessary to determine if sinuses/tracts communicate with the anal sacs.
If the patient is a German shepherd, anal furunculosis is most often diagnosed on the basis of clinical presentation and physical examination alone. If the dog is another breed, other causes based on clinical signs should be ruled out first. For example, anal sac infection/abscess, cancer, allergies, foreign body, etc should be considered for breeds other than the GSD.
Treatment and management of anal furunculosis
Timely diagnosis and appropriate, lifelong therapy are critical. Lack of or unsuccessful treatment for any length of time carries the potential for development of anal stricture and large, deep draining tracts (furuncles), which decrease the patient and owner’s quality of life and can lead to owner’s electing to euthanize a pet.
Over the past 6 decades, a wide variety of treatments for anal furunculosis have been used. Surgical treatment is no longer recommended as it has been shown to result in a high incidence of severe complications (fecal incontinence, diarrhea, rectal stricture, wound dehiscence and severe pain/suffering) and lack of resolution. Immunosuppressive therapy is the mainstay of treatment and 99.5% of dogs experience significant improvement to a manageable state with most dogs enjoying resolution of the disease. Lifelong treatment is necessary with adjustments needed at times if recurrence is noted.
Immunosuppressive Therapy
A wide variety of immunosuppressive therapies, as either single or combination therapy, have been used to treat anal furunculosis. Almost all patients require long-term immunosuppressive treatment to keep the disease in remission. Therefore, patients should be evaluated periodically for potential side effects. Medications range from those given by mouth to topically applied to the affected area on and around the anus – this is called the perineal region.
Generally, moderately to severely affected animals will be started on topical and oral medication until the lesions are healed and then maintained on topical medication. For more severely affected animals, topical therapy is not enough to keep the disease in remission so they will require tapering oral medications to the lowest effective dose and continuing topical meds for their lifetime. Occasionally the disease is severe enough that multiple oral medications, topical treatments and surgery for anal sac removal are all indicated. Flare ups may also occur and can require starting induction therapy with oral and topical medications, potentially antibiotics if secondary infection if present.
Treatment For Concurrent Food Allergies
A link between anal furunculosis and adverse food reactions has been identified. In one study, 18.8% of dogs with anal furunculosis also had food allergies.19 Whether there is a direct correlation (ie: association) between the diseases or the dogs studied happened to have 2 diseases at once is not known. Regardless, use of a novel protein diet or hydrolyzed diet can be beneficial for some patients.
Remission Of Anal Furunculosis
Depending on instituted treatments and owner compliance, most patients will start to show clinical improvement within a few weeks. The furuncles may not be completely healed, but other clinical signs should improve. Almost all dogs require lifelong therapy to keep the disease in remission.
Conclusion
Anal furunculosis can be a severely debilitating disease. Most dogs respond well to multimodal therapy if initiated in a timely fashion. The more severe the disease, the more aggressive initial therapy needs to be, including combination therapies.
Modified for educational purposes only from: Perianal Fistulas in Dogs accessed 7 AUG ‘24
Cain CL. Canine Perianal Furuncles: Clinical Presentation, Pathogenesis, and Management. Vet Clin North Am Small Anim Pract. 2019 Jan;49(1):53-65. doi: 10.1016/j.cvsm.2018.08.006. Epub 2018 Sep 11. PMID: 30213533.

